Inflammatory Bowel Disease has a direct link with the gastrointestinal (GI) tract, Crohn’s disease, and ulcerative colitis. IBDs are characterized by inflammation or immune activation within the gastrointestinal tract. Its prevalence is increasing day by day and is the dominant disease in developed countries. Its incidence is becoming higher in Western countries, including the United States, Canada, and Europe where one million, two million, and two and half million people are estimated to have IBDs, respectively.
Although IBD is not fatal, it badly affects the quality of life by causing diarrhea, vomiting, and severe pains. Its most hazardous risk is colorectal cancer. This article will help you to understand the immunological, infectious, and psychological factors causing IBD, their prevention, and cure.
Definition of IBD
IBD refers to two common diseases of the intestinal tract– Ulcerative colitis and Crohn’s disease. The former causes disease in the large intestine while the latter causes damage to any part of the gastrointestinal tract from mouth to anus. There is an indeterminate form of both known as the third category, called IBD. It has a combination of features of both Crohn’s disease and Ulcerative colitis.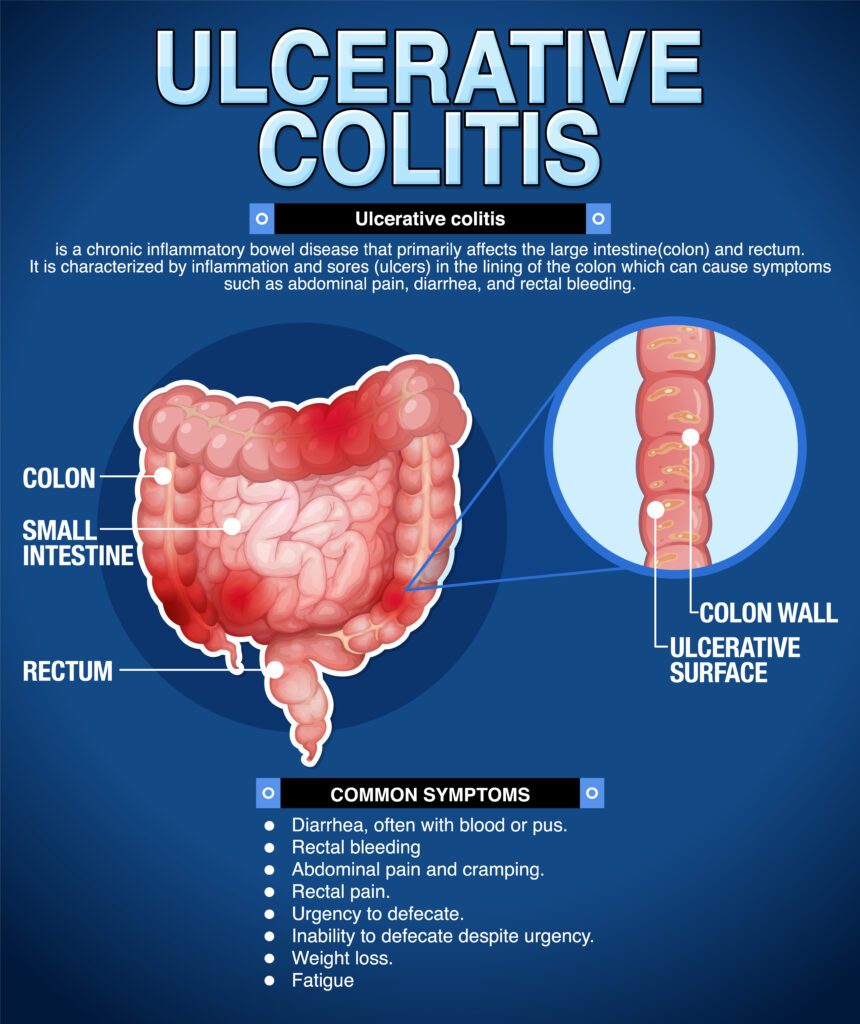
Prevalence and Impact of IBD on Individuals
According to an estimate 1.6 million Americans are affected by IBD. This is an autoimmune disorder in which the body’s immunity fights against healthy tissues and attacks them. The actual causes or triggers of these attacks are still under discussion and not known. Researchers are still working to explore the mechanisms and conditions that generate factors to attack healthy tissues. Studies reveal that the balance of bacteria in the gut, and environmental and genetic triggers contribute to IBD. It is also suggested that IBD is a hereditary disease but it also can be developed randomly.
Antibiotic Use and its Relationship with IBD Risk The use of antibiotics was associated with an increased risk of IBD development. Medicines used to treat gastrointestinal tract infections enhance the risk of developing IBD. but the only exception is nitrofurantoin, the medicine prescribed for the treatment of urinary tract infection and is not linked with IBD developing risk.
The use of antibiotics was associated with an increased risk of IBD development. Medicines used to treat gastrointestinal tract infections enhance the risk of developing IBD. but the only exception is nitrofurantoin, the medicine prescribed for the treatment of urinary tract infection and is not linked with IBD developing risk.
Research Findings on the Association between Antibiotics and IBD
According to new studies, the frequent use of broad-spectrum antibiotics increases the risk of developing inflammatory bowel disease. A recent research conducted in Sweden suggested that the United States, Europe, and other developed countries have an increasing number of IBD patients due to the frequent use of antibiotics for treating infections. These antibiotics have hazardous impacts on the gut and lead to gastrointestinal disease by altering fragile microbial communities in the gut. So you may conclude that higher cumulative exposure to systemic antibiotic therapy appears to be strongly associated with a greater risk of new onset of IBD.
Factors Contributing to the Link between Antibiotic Use and IBD Risk
According to new studies nearly seven million people are diagnosed with IBD or the main types i.e. Crohn’s disease or Ulcerative colitis. Environmental factors, genetics, and family history are major factors but the use of antibiotics at an early age is also a major cause of developing IBD. The use of antibiotics for age, sex, or socioeconomic status reduces stomach acidity and alters the microbiome thus increasing the risk of IBD. People in the age group 10 years to 40 years are at higher risk of developing IBD.
Epidemiological Studies Supporting the Connection between Antibiotics and IBD Development
Disease is prevailing in some specified regions of the world, this fact drags us to study epidemiological trends to explore the environmental factors that play crucial roles in the pathogenesis of Crohn’s disease and Ulcerative colitis. However, to find the major factors for the prevalence of Inflammatory Bowel Disease (IBD), the genetic factor is also under observation. Studies also reveal that an inappropriate immune activation also supports the intestinal barriers to cause IBD.
Mechanism of IBD Risk
By observing clinical and endoscopic findings observed in patients of IBD we have gathered some information to suggest the mechanism of IBD development from genetic, environmental, intestinal barriers, and immunologic perspectives. Let’s have a deep look to understand.
Genetic Factors: CD and UC seem to be inheritable and the risk for disease development in first-degree relatives of patients is up to 5 folds higher than that in healthy people. A deep study of the family history of patients with IBD has helped researchers identify the rare genetic variants that interfere with pathways that cause intestinal inflammation. Studies suggest that this is a polygenic disease because multiple common genetic polymorphisms drive it.
Environmental Factors: New epidemiological trends of IBD suggest that environmental factors enhance the risk of promoting intestinal inflammation.
Smoking is the most observed risk factor that is harmful for patients of CD but protective for UC patients. In addition, the use of a diet rich in saturated fatty acids also increases the risk but a high-fiber diet reduces the risk. Frequent use of medicines, mostly antibiotics, has been strongly associated with increased risk factors. Some modes of life including infections, exposure to pets, and breastfeeding are considered as greater risk for the development of IBD. The intestinal microbiome is a strong connection between the intestinal mucosa and the outside environment. This microbial dysbiosis causes a decrease in the diversity of microbiomes leading to IBD.
The Intestinal Barrier: Luminal content and intestinal mucosa exist in an equilibrium state but the disturbance in this equilibrium may lead to IBD. Epithelial cells of the intestine and innate immune cells are responsible for maintaining this equilibrium. The imbalance in this combination can cause IBD.
Impact of Antibiotics on Gut Microbiota Composition
The use of antibiotics reduces the diversity of microbiota in the gut resulting in the loss of important taxa causing the development of bacterial antibiotic resistance. Frequent use of antibiotics at an early age results in an increase in the prevalence of Enterobacteriaceae and some other pathobionts with a greater decrease in Bifidobacterium which are essential species for gut health.
Disruption of Microbial Balance and Its Consequences on Intestinal Health
Several mechanisms are involved in maintaining the homeostasis of intestinal epithelium such as the thickness of the mucus layer and tight junctions. Normal gut microbes are eliminated due to exposure to antibiotics that disrupt the microbial balance and harm the intestinal health by decreasing secretion of microbial peptides. In addition, thinning of mucus layer makes intestinal epithelium more susceptible to damage. Variations in microbial protease also affect mucosal barrier function. In conclusion, all these processes facilitate the invasion of enteric pathogens.
Influence of Antibiotic-Induced Dysbiosis on Immune System Function
Disturbance in natural microbial communities due to the use of antibiotics induced dysbiosis on immune system function and modulates immune system functions that promote illnesses associated with dysfunctional immune systems. Use of antibiotics when you feel sick is correlated with an increased risk of various infections, asthma, and IBD.
Evidence Supporting Antibiotic-Induced Dysbiosis in IBD
During early childhood, the increased exposure to antibiotics increases the risk of antibiotic-induced dysbiosis in IBD many fold which is the result of reduction in diversity of specific microbial species and abundance of some unnecessary taxa. This may cause an emergence of antibiotic-resistant microbes and disruption of host immunity. All of these processes are linked with the development of immune-related and metabolic disorders. The administration of antibiotics predisposed to gut microbiota dysbiosis including obese children and newborns. Resulting in negative health outcomes.
Studies Demonstrating Alterations in Gut Microbiota Following Antibiotic Use
Gut microbiota get maturation after the first five years of life, and exist as a stable ecosystem in healthy people. Alterations of various types however occur at different stages of life in response to different stimuli such as living conditions, diet, and use of medicinal drugs. Studies show that human gut microbiota is variable but recovers after drastic pulse perturbations like courses of antibiotics. Managing a robust microbiome is crucial for limiting the period of microbial destruction due to the use of antibiotics. Diet, environmental factors, past perturbations, and specific characteristics of antibiotics are recognized as the major factors that may help to recover the human gut biota’s initial composition.
Identification of Specific Bacterial Species that Affect IBD Patients
Here is a list of specific bacterial species that affect IBD patients.
Clostridium difficile: This species increases the permeability of epithelial tissues and causes luminal fluid accumulation. It also causes epithelial cell death.
Mycobacterium avium: This species is responsible for binding M cells through fibronectin.
Paratuberculosis (MAP): Its micro bacterial products scavenge reactive oxygen intermediates and proliferate between macrophages.
Fusobacterium varium: This species is responsible for producing a high level of n-butyric acid in bacterial culture that kills Vero cells.
Implications for Clinical Practice and Future Research
Therapeutic options for the patients of IBD are expanding rapidly but the factors present that play a role of barriers to proceedings. Patients with inflammatory bowel diseases face some hurdles that prevent them from benefiting from the advances made in clinical practices to treat IBD. Prescribed drugs, prior authorization, and step therapy are the major barriers but inadequate multidisciplinary care is also a prevailing cause that limits the patient’s access to high-quality care. However, the opportunities to access high-quality care still exist. This can be done by the collaborative working of patients, providers, and payers.
Recommendations for Judicious Antibiotic Use in Patients at Risk for IBD
Inflammatory bowel disease is a diverse condition with a response to treatment dependent on interrelated variables. To understand the risk of antibiotics in IBD as a whole is overly simplistic and may not reflect the true effect in specific circumstances. Therefore, an attempt is made to review the role of antibiotics in more specific scenarios.
Due to the lack of high-quality studies in antibiotics, it is difficult to describe the treatment courses, and outcome measures and draw firm conclusions. Therefore, it is concluded that the efficacy of therapeutic interventions generally depends on several large, high-quality controlled trials i.e. RCTs.
Areas for Further Investigation to Better Understand IBD Diagnosis
Inflammatory bowel disease is a disease that still needs more investigations and studies to characterize the typical findings associated with it. Barium enema imaging technique is one of the first studies in this regard and it is considered useful in case of limited or no access to endoscopy. It may also be used in case of incomplete colonoscopy to measure stricture length. Generally, doctors use biopsies during a colonoscopy to remove small tissues from the colon to test in the laboratory. Biopsy results help them to confirm IBD and to differentiate between Crohn’s disease and Ulcerative colitis. In addition, some latest technologies including magnetic resonance imaging (MRI), computed tomography (CT), and Ultrasound(US) are also used to diagnose IBD. Recent research has confirmed that IBD is commonly diagnosed between 30 to 35 years old people and the second peak time of symptom appearance is 50 to 60 years. It usually appears as a sudden flare-up of symptoms. However, there is no single test to diagnose IBD.
Conclusion
Inflammatory bowel disease refers to long-standing inflammation of tissues in your digestive tract. Both types of IBD involve sores along the lining of your large intestine and rectum. Diagnostic results inform you that your immune system is causing inflammation indicating that you are anemic with a low number of red blood cells which may be the result of internal bleeding. Following a residue diet may help to relieve abdominal pain but in case of having strictures, you should avoid nuts, fruits, and vegetables. Use cold foods to prevent diarrhea. Treatment of disease involves drug therapy or surgery.
IBD is a disease that evolved from a fatal disease to a manageable chronic condition with two emerging forms. Now in the era of scientific advancements and progressive technology, the etiology of IBD and its treatment is becoming more precise and continues to increase with time.